The deadly epidemic you’ve never heard of
Valley Fever cases rise as climate change creates more hot spots for the deadly spores.
Story and photos by Adam Ernesto Fuentes
I have never been one to stay still for too long. During holidays or in between school semesters, I would jump in my Pontiac, recruit a few friends and drive out into the Mojave Desert. My windows were always down, my music was always loud, and my arm was stretched out into the wind as I drove through California’s Central Valley. The Interstate 5 Highway cuts across lowly fields of apricots, grapes, almonds and figs. The horizon is muddied by wind-swept dust blown from the arid land. It was only recently that I became aware that every drive, every breath I took, could have killed me. It could still kill me, and quite possibly, has already begun.
The California dust holds a deadly secret, one that has been plaguing the American Southwest for over a century. Killer microscopic fungal spores called Coccidioidomycosis, simply known as Cocci, or Valley Fever, are too small to be detected even by the most advanced bioterrorism equipment in the country. It causes a lottery of symptoms to anyone unlucky enough to breathe the contaminated dust endemic to the American Southwest: California, Nevada, Arizona and New Mexico; Northern Mexico; Central America; and parts of South America. The Center for Disease Control CDC estimates that about 150,000 people are infected yearly in the United States alone. About 60 percent of its victims show no symptoms whatsoever. Those that do show symptoms experience fever, cough, headaches, fatigue, muscle aches, and joint pain often misdiagnosed as the common flu, bacterial pneumonia, and even cancer.
Valley fever begins its life in the soil. During wet seasons the fungus multiplies but remains trapped in the moist dirt. When dry weather turns the soil arid, the spores carry off into the wind. When the spores are inhaled, they multiply into sphere-like structures that feed on the warm, moist tissues of the lungs. The disease kills between 200–500 Americans every year. Only California, Arizona, Nevada, New York, and Rhode Island are required to report the number of infections. Because the disease is largely misdiagnosed, the number of deaths from Valley Fever could be in the thousands nationwide.
“It destroys lives. Divorces, lost jobs and bankruptcy are incredibly common, not to mention psychological dislocation,” said Dr. Royce Johnson in a New York Times article in July.
Johnson is an infectious disease specialist and Valley Fever expert who became involved after his daughter contracted the disease. Johnson’s medical office is located in Bakersfield, Calif., one of the hot spots for Valley Fever.
One single spore is enough to contract the disease. In frequent cases the infection turns into a lifelong fight for survival.
Valley Fever has no cure, and whether you are asymptomatic or have a severe case, the fungus, like HIV, never goes away.
Regardless of your age, physical condition, sex or race, Valley Fever does not discriminate. The simple act of breathing is the most common way to become infected. The California Department of Public Health states on its website: “Although it can be difficult to prevent Valley Fever, the best way to reduce your risk is to avoid breathing in dirt or dust in areas where Valley Fever is common.” There are four million people living in the at-risk areas of the American Southwest. For these residents and tourists, avoiding contact with the dust is nothing short of impossible.
In 3 to 5 percent of the infected population the fungus disseminates to various parts of the body such as the skin, bones, joints, liver, heart and the lining of the brain causing Cocci meningitis. At the age of 2, Julia Buckley was an active little girl from Fountain Hills, Ariz. who loved to dance. When she contracted Valley Fever, it went unnoticed. As the fungus began to multiply in her lungs, Valley Fever manifested itself in its deadliest form. Her mother, LeAnn Buckley, explained: “She was throwing up every 30 minutes. I took her to the hospital and it took about a week to figure out what was wrong with her. They found the Valley Fever in her cranial fluid.”

Disseminated Valley Fever in the brain is the most lethal complication. Julia was given a 30 percent chance of survival and spent three months in the intensive care unit.
“I think I cried every day at the hospital,” said her mother. Julia survived the meningitis infection and her Valley Fever went into remission. The anti-fungal medication Flucanazole she takes can be just as debilitating as the illness itself. Buckley recalled how every four months her daughter had to be tested for liver damage due to the side effects of the medication. “They recommend that she stay on it for the rest of her life because if she gets off of it, she might have a flair up again,” explained her mother.
Buckley does not qualify for medical insurance and has to pay out of pocket for her daughter’s medical expenses. Now Julia is 8 and attends elementary school. She suffers from constant exhaustion and often has to miss school due to pain in her arms and legs.
There are certain groups of people at a higher risk for disseminated Valley Fever: African-American or Filipino males, women in their third trimester of pregnancy, and anyone with diabetes or a compromised immune system such as HIV/AIDS or an organ transplant recipient.
If you are not holding your breath by now, or at the very least wondering why you have never heard of Valley Fever, you are not alone. Most people only hear about it once they have been affected by it. It is a proximity disease; it’s the Southwest’s best-kept secret. I asked Buckley how she might explain the reason why there is no national awareness of the disease that almost claimed the life of her daughter. She said it all comes down to private interest.
“The state of Arizona is based on tourism; they keep telling people about Valley Fever and [tourists] might not want to come here on vacation.”
The travel site www.visitarizona.com calculates that 37 million international and domestic tourists made the state their travel destination generating roughly $500 million in state revenue. There are more cases of Valley Fever in Arizona than anywhere else in the world, followed by the San Joaquin Valley of California where millions unknowingly put themselves at risk by commuting through the central valley on Interstate 5 every year.
It is unclear why certain diseases generate more fear and national attention than others. Perhaps, the areas it infects or the people that fall prey determine a disease’s popularity. In 1999, the West Nile Virus made its first appearance in American soil. The virus crossed the Atlantic Ocean into New York City and over a period of five years, spread across the United States. Between 1999 and 2012, there were 37,088 cases according to the CDC. Print and broadcast media coverage of the virus was prevalent and so was public concern.
Over $54 million in funding has been raised to prevent the spread of West Nile and find a cure. Yet in 2011, there were more than 22,000 cases of Valley Fever in the United States. More cases of the fungus were reported in that year alone than in the entire history of West Nile in America. Still, funding for a Valley Fever vaccine is only 4 percent that of West Nile.
There is a reason why this disease should matter to everyone — it’s spreading. In 2001, three residents of Washington State were diagnosed with Valley Fever and each victim reported no recent travel outside of the state. In an investigation by the CDC, Valley Fever was found growing in the south central part of the state. The samples in the soil matched the DNA of the fungus taken from a patient, further proving that the disease was contracted in the state of Washington.
Valley fever is largely a blue-collar disease with workers in construction, agriculture, ranching, archeology, and military fields employed in the Southwest at a severe risk of infection. California native Jeffrey Smith, 38, worked as a landscaper in Orange County south of Los Angeles before moving to Maine. At 20, he enlisted into the California Conservation Corps to gain experience working in nature and the outdoors. He was deployed to Bakersfield to clean up abandoned house lots in low-income neighborhoods. In Stockton, Calif. he helped prevent floods and worked to build an aquifer in Porterville, Calif. This year, he consulted his doctor about a series of symptoms that had persisted for almost three years.
“I thought for the longest time I had Lyme disease but never tested positive,” he said. It was a series of new symptoms that motivated him to seek medical attention. Smith started to experience shortness of breath, chest pain, and blood when he coughed. After several X-rays and a bronchoscopy, Smith was misdiagnosed with a Klebsiella bacterial infection. He was put on steroids and antibiotics but he quickly was admitted to the hospital with a fever of 104. The misdiagnosis allowed the Cocci fungus to spread throughout both of his lungs before he was properly diagnosed with Valley Fever. Like so many others, Smith will have to be on medication for the rest of his life in order to keep the fungus under control. The illness has left him with peripheral neuropathy and degenerative neck complications. Smith is one of many examples of how misinformation in the medical community can delay a proper diagnosis with devastating consequences to the patient. Looking back at his time in the CCC it is difficult for Smith to pinpoint exactly where he might have been infected.
“I really don’t know where I got Valley Fever. I lived all over California for many years so it could have been anywhere,” Smith said.
No major studies have been conducted on the effect that climate change has on the spread of Valley Fever, but one thing is very certain, Valley Fever is a growing epidemic. Hotter weather may cause Valley Fever to thrive outside of the current endemic areas and create new hot spots for the fungus. The CDC reports that the number of cases in California has increased by 850 percent in recent years. The number of cases in the Southwestern states rose from 2,265 in 1998 to 22,401 by 2011. It is still not yet clear how and why valley fever spreads, but current drought conditions, increased construction, and population booms in endemic areas are all relatable causes. Extreme winds have been known to blow the Cocci spores well over 500 miles away from its endemic source.
Valley Fever in California is now being reported in areas outside the Central Valley and in more temperate environments. Dr. Michael Albertson, a gastroenterologist at UCLA who lived in Woodland Hills, located in the San Fernando Valley of Los Angeles County, nearly lost his life to Valley Fever when the disease manifested itself as a deadly combination of pneumonia and a hyper allergic reaction to the fungus. In October of 2010, Albertson developed a fever and a cough that persisted for over a week. An X-ray of his chest revealed pneumonia in his left lung. His physician diagnosed him with bacterial pneumonia and prescribed a treatment of antibiotics, but by Sunday night he was rushed to the hospital with a high fever.
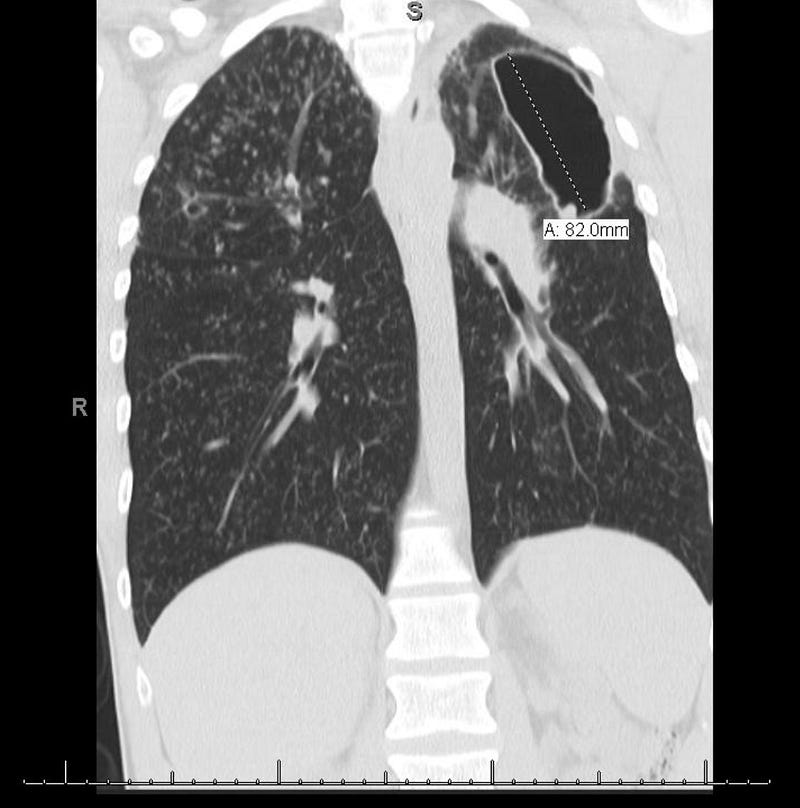
The following Monday, a second chest X-ray uncovered the spread of the pneumonia to his other lung. By Wednesday, unable to breathe, he was attached to a ventilator and placed in the intensive care unit. His doctor treated the pneumonia with corticosteroids and antibiotics, and Albertson improved and was released from the hospital. As his corticosteroid medication was decreased, the pneumonia mysteriously returned and he was back in ICU with dangerously low blood oxygen and blood pressure levels. What transpired from that point on was a rush to save his life as his lungs filled with fluid. On full support to breathe and two negative tests for Valley Fever, the third finally came back positive. Antifungals were started but Albertson continued to get worse.
“Without the ventilator, I would have died. My family expected me to die at the hospital,” Albertson said.
No one could understand why the medication meant to combat the disease was further crippling his health. The entire mystery loomed over Albertson’s life as if death itself had manifested into the room.
“It was like something out of the show, House,” recalled his wife, Toni Albertson, a professor of journalism in Los Angeles. “I was watching my husband die and no one could figure out why.”
She took her husband’s stark prognosis as her own cause for intervention and searched through support groups and medical websites for answers. She asked UCLA pulmonary research specialist Dr. Michael Roth, who had come on for a two-week rotation, why her husband had improved while on steroids. This prompted Roth to do some research and return with an obscure study on eight patients who had contracted Cocci pneumonia that developed into a hypereosinophilic reaction; in other words, an allergic reaction to the Cocci. The patients in the study were treated with steroids. Of those patients, only one had survived. The doctors now faced a difficult choice. They knew that treatment of Valley Fever with steroids could have adverse consequences, but his wife pressed on and urged the doctors to change her husband’s medication. “He was dying anyway. It was our only option,” she said.
They shot him full of steroids and within 24 hours, his lungs cleared and within 48 hours, he was breathing without machines.“It was like watching ice melt,” his wife said about the improvement of his X-rays.
What followed was a long and slow recovery that included intense physical therapy before he could be well enough to return to work. He had lost 40 pounds and could not walk without assistance. Although it has been four years since Albertson nearly lost his life, Valley Fever remains a constant risk to his health. “The illness is a devastating illness; it never goes away and it’s always in your body,” warns Albertson. “I am on medication and I will be on it for possibly the rest of my life.”
Albertson is monitored through regular Cocci titer blood tests to make sure the fungus remains inactive. “Hopefully the titers will be down to zero and they’ll stay at zero but there is no way to predict that,” Albertson said.
The Valley Fever Center for Excellence, located at the University of Arizona, reported earlier this year that it may have a possible cure. Several pharmaceutical companies had attempted to find a cure before but failed or gave up all together because the market for the drug is very small and therefore not profitable. The University of Arizona has since taken up the task of pursuing a cure funded by various research grants. Funding for the cure now totals $7.5 million, but according to the university, tens of millions of dollars are needed to approve and manufacture the cure. Clinical trials are expected to start this year or early 2015.
Until a cure is found and Valley Fever contained, many victims and family members will continue to seek answers. Support groups like valleyfeversurvivor.com are beacons of information. They are instrumental in providing a community where people can share their experiences and find some comfort and hope.
As for me, I can’t say I am a survivor. I can’t say my family has suffered like many others from this tiny fungus with a great power to change the course of someone’s life. We are always moving, working, driving, and in my case with the windows up from now on. Valley Fever matters because all it takes is one tiny spore, and one deep breath.
Substance is a publication of the Mt. San Antonio College Journalism Program. The program recently moved its newsroom over to Medium as part of a one-year experiment. Read about it here: https://medium.com/substance/the-experiment-be947b2ba13e